Nature’s most feared creatures often carry the most unexpected gifts. While most of us instinctively swat away wasps, scientists are discovering that these seemingly aggressive insects might hold the key to treating one of humanity’s most devastating diseases. Deep within the venom of certain wasp species lies a potent toxin that could revolutionize breast cancer treatment, transforming our understanding of how natural compounds can be harnessed for medical breakthroughs.
The Unlikely Hero: Polybia Paulista

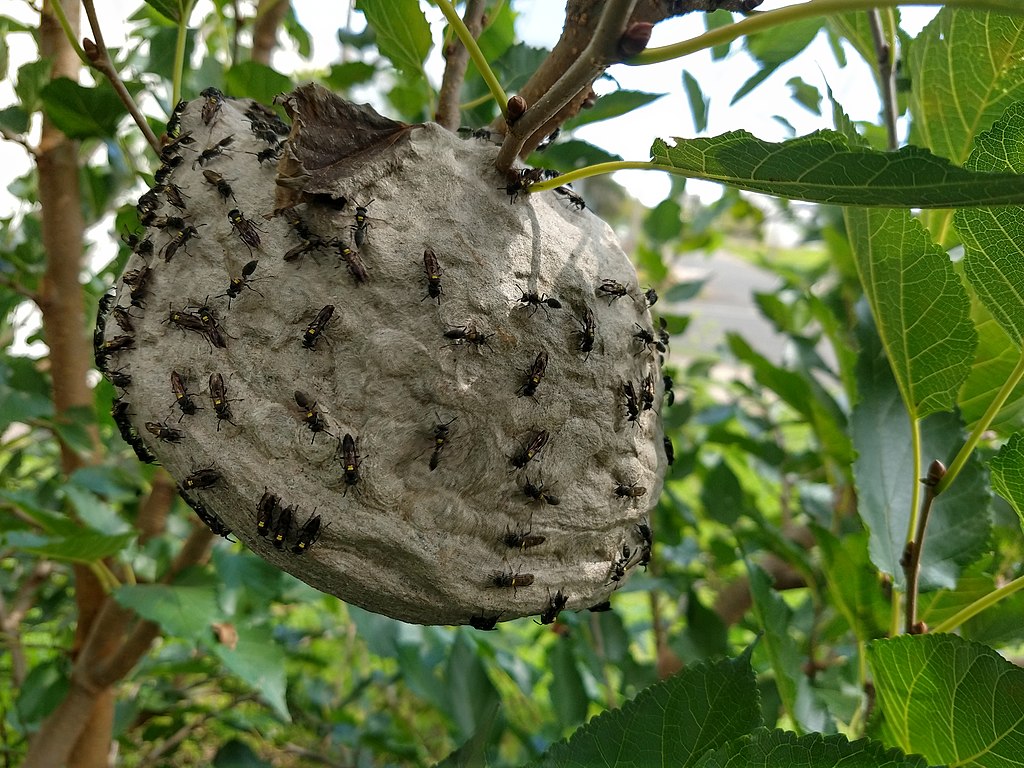
The Brazilian social wasp Polybia paulista doesn’t look like a medical marvel. This small, brownish wasp buzzes around South American forests, building paper nests and defending its colony with fierce determination. Yet hidden in its venom sac is a peptide called MP1 that has captured the attention of oncologists worldwide.cMP1 stands for “Mastoparans Polybia-1,” a name that barely hints at its extraordinary potential. This peptide consists of just 14 amino acids arranged in a specific sequence that gives it remarkable properties. When researchers first isolated this compound, they had no idea they were looking at a potential game-changer in cancer therapy.
How Nature’s Weapons Target Cancer Cells

The mechanism behind MP1’s cancer-fighting abilities reads like something from a science fiction novel. This wasp toxin specifically targets the outer membrane of cancer cells, exploiting a fundamental difference between healthy and malignant tissue. Cancer cells have altered membrane compositions that make them vulnerable to MP1’s attack, while normal cells remain largely unaffected. Think of it like a master key that only opens certain doors. MP1 recognizes the unique molecular signature of cancer cells and binds to specific lipids in their membranes. This binding triggers a cascade of events that ultimately leads to cell death through a process called apoptosis. The selectivity of this process is what makes MP1 so promising. Traditional chemotherapy drugs often damage healthy cells alongside cancerous ones, causing the debilitating side effects that cancer patients know all too well.
Breaking Down the Science: Membrane Selectivity

The secret to MP1’s effectiveness lies in the composition of cancer cell membranes. Healthy cells maintain a careful balance of phospholipids, with negatively charged lipids primarily on the inner leaflet of their membranes. Cancer cells, however, lose this asymmetry, exposing negatively charged phosphatidylserine and phosphatidylethanolamine on their outer surface. MP1 is positively charged, creating an electrostatic attraction to these exposed negative charges on cancer cells. This molecular recognition system allows the peptide to distinguish between friend and foe at the cellular level. Once bound, MP1 can disrupt the membrane integrity or trigger programmed cell death pathways.
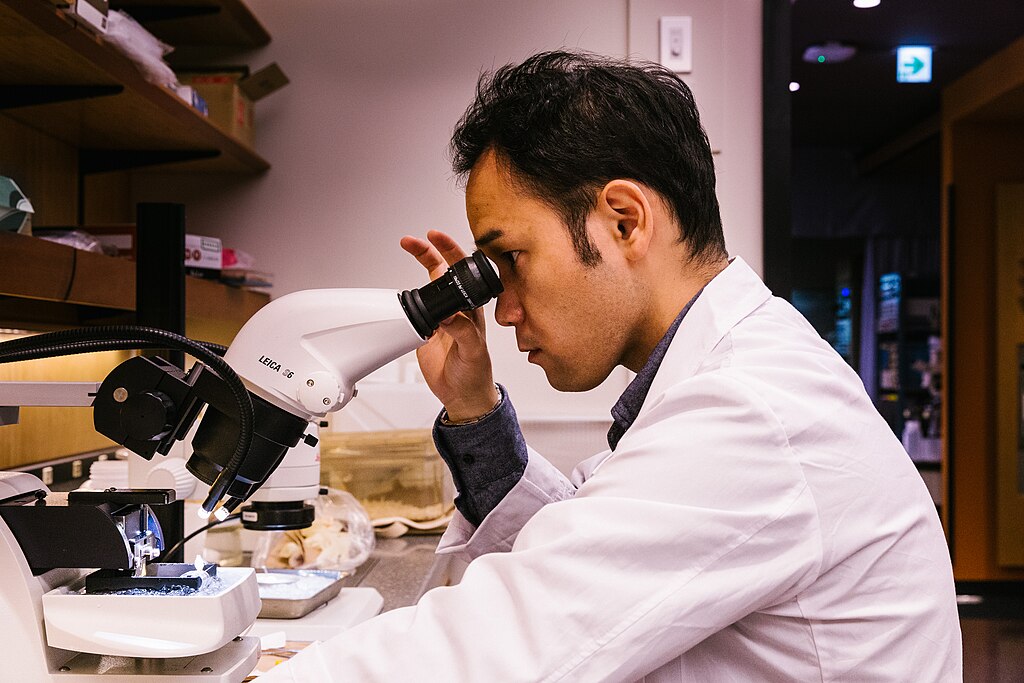
Laboratory Breakthroughs: From Petri Dish to Promise

Initial laboratory studies with MP1 have yielded results that even seasoned researchers describe as remarkable. In cell culture experiments, the wasp toxin demonstrated potent activity against various breast cancer cell lines while showing minimal toxicity to normal breast tissue cells. The therapeutic window – the difference between effective and toxic doses – appears to be significantly wider than many current cancer drugs. Researchers have observed that MP1 can induce cancer cell death through multiple pathways simultaneously. Some cells die through membrane disruption, while others undergo apoptosis triggered by the peptide’s interaction with specific cellular targets. This multi-modal approach could make it harder for cancer cells to develop resistance, a major challenge in current cancer treatment.
Animal Studies: Promising Results in Living Systems

The transition from laboratory dishes to living organisms marked a critical milestone in MP1 research. Animal studies using mouse models of breast cancer have shown encouraging results, with tumors shrinking significantly following MP1 treatment. Even more promising, the treated animals showed fewer side effects compared to those receiving conventional chemotherapy. In one particularly striking study, mice with aggressive breast tumors showed a 60% reduction in tumor size after MP1 treatment. The peptide appeared to work synergistically with the animals’ immune systems, not only killing cancer cells directly but also stimulating immune responses against the tumors. These studies also revealed that MP1 could potentially overcome some forms of drug resistance that plague current cancer treatments. Even tumors that had become resistant to conventional therapies showed sensitivity to the wasp toxin.
The Challenge of Drug Development

Despite its promise, transforming MP1 from a laboratory curiosity into a viable cancer treatment faces significant hurdles. Peptides like MP1 are notoriously difficult to work with as drugs – they’re quickly broken down by enzymes in the body, have trouble crossing biological barriers, and can trigger immune responses. Researchers are exploring various strategies to overcome these challenges. Some are modifying the peptide structure to make it more stable while preserving its anti-cancer activity. Others are developing delivery systems that could protect MP1 from degradation while targeting it specifically to tumor sites. The manufacturing process for peptide drugs is also more complex and expensive than traditional small-molecule drugs. This reality could impact the eventual cost and accessibility of MP1-based treatments if they reach the market.
Synthetic Biology: Engineering Better Toxins

Modern biotechnology is opening new possibilities for optimizing MP1’s therapeutic potential. Scientists are using synthetic biology techniques to create modified versions of the peptide that retain its cancer-fighting properties while improving its drug-like characteristics. These synthetic analogs might be more stable, less immunogenic, or more specifically targeted to certain cancer types. Computer modeling and artificial intelligence are accelerating this process, allowing researchers to predict how different modifications might affect MP1’s behavior without having to test every possibility in the laboratory. This approach could significantly speed up the development timeline for new MP1-based therapies.
Combination Therapies: Amplifying the Impact

One of the most exciting prospects for MP1 lies in its potential use alongside existing cancer treatments. Preliminary studies suggest that the wasp toxin might work synergistically with immunotherapy drugs, radiation therapy, and even some chemotherapy agents. This combination approach could allow for lower doses of each treatment while maintaining or even improving overall effectiveness. The unique mechanism of MP1 means it could theoretically be combined with almost any other cancer treatment without competing for the same cellular targets. This flexibility could make it a valuable addition to the cancer treatment arsenal, regardless of other therapeutic advances.
Beyond Breast Cancer: Broader Applications

While much of the research focus has been on breast cancer, MP1’s mechanism of action suggests it could be effective against other cancer types as well. The altered membrane composition that makes cancer cells vulnerable to MP1 is not unique to breast cancer – it’s a common feature of many malignant cell types. Early studies have shown promise against prostate cancer, bladder cancer, and certain blood cancers. The peptide’s ability to target cancer stem cells – the resilient cells that often drive tumor recurrence – is particularly intriguing for researchers studying drug-resistant cancers. Some researchers are even exploring MP1’s potential in treating non-cancerous conditions characterized by abnormal cell growth or inflammation, though cancer remains the primary focus of development efforts.
The Wasp’s Evolutionary Advantage

Understanding why wasps evolved such a potent toxin provides insight into its mechanism and potential applications. MP1 likely evolved as a defensive weapon against the wasp’s natural enemies, particularly other insects and small predators. The peptide’s ability to disrupt cell membranes would be highly effective against a wide range of threats. This evolutionary perspective also explains why MP1 shows selectivity for certain cell types. In nature, the toxin needed to be potent enough to deter threats while not being so broadly toxic that it would harm beneficial insects or contaminate the wasp’s own environment. The fact that millions of years of evolution have refined this molecular weapon gives researchers confidence that MP1 represents a genuinely optimized biological tool that could be adapted for human medicine.
Regulatory Hurdles and Clinical Trials
The path from promising laboratory results to approved cancer treatment is long and carefully regulated. MP1 will need to undergo extensive safety testing before it can be tried in human patients. The first human trials will likely focus on safety and dosing rather than effectiveness, following the standard phases of clinical development. Regulatory agencies like the FDA and EMA will require comprehensive data on MP1’s toxicity, pharmacokinetics, and manufacturing quality before approving clinical trials. The unique nature of the compound – being derived from wasp venom – may require additional safety studies to address potential concerns about allergic reactions or other immune responses. The clinical development process typically takes 10-15 years and costs hundreds of millions of dollars. However, the promising preclinical results with MP1 have attracted the attention of pharmaceutical companies and research institutions willing to invest in its development.
Environmental and Ethical Considerations

The potential medical applications of MP1 raise important questions about the conservation of wasp species and their habitats. If this toxin proves successful as a cancer treatment, there could be pressure to harvest wasps or their venom on a commercial scale. However, most researchers are focusing on synthetic production methods that wouldn’t require large-scale wasp harvesting. The Brazilian forests where Polybia paulista lives are under constant threat from deforestation and development. The discovery of MP1’s medical potential adds another compelling reason to protect these ecosystems – they may contain countless other compounds with therapeutic potential that we haven’t yet discovered. This situation highlights the broader importance of biodiversity conservation for human health and medicine. Many of our most important drugs have natural origins, and the loss of species and habitats could eliminate potential cures before we even know they exist.
The Future of Venom-Based Medicine

MP1 represents just one example of how venoms and toxins from various species are being investigated for medical applications. Snake venoms have already provided several important drugs, including medications for high blood pressure and diabetes. Spider venoms are being studied for their potential in treating chronic pain and neurological conditions. The field of venomics – the study of venoms for drug discovery – is rapidly expanding as researchers develop better tools for analyzing these complex molecular cocktails. Each venom contains dozens or even hundreds of different compounds, many of which have never been studied for their therapeutic potential. Advanced screening technologies and computational biology are accelerating the pace of venom-based drug discovery. What once took years of painstaking chemical isolation and testing can now be accomplished in months, opening up new possibilities for finding medical applications for these natural toxins.
Looking Ahead: Hope and Realistic Expectations
The story of MP1 embodies both the incredible potential and the sobering challenges of modern drug development. While the early results are undeniably encouraging, the history of medicine is filled with promising compounds that failed to live up to their initial promise. The transition from laboratory success to clinical reality is fraught with unexpected obstacles and setbacks. Yet the unique properties of MP1 – its selectivity for cancer cells, its multiple mechanisms of action, and its potential for combination with other treatments – suggest that this wasp toxin might succeed where others have failed. The growing understanding of cancer biology and improvements in drug delivery systems create a more favorable environment for peptide-based therapies than existed in the past. Even if MP1 doesn’t become the breakthrough cancer treatment that researchers hope for, the knowledge gained from studying this compound will undoubtedly contribute to future advances in cancer therapy. Each failure teaches valuable lessons that bring us closer to success.
Conclusion
The next time you encounter a wasp, you might pause to consider the remarkable potential hidden within its tiny venom sac. These insects, often dismissed as mere nuisances, may hold keys to treating diseases that have plagued humanity for millennia. The intersection of nature’s ancient wisdom and modern medical science continues to yield surprises that challenge our assumptions about where the next breakthrough might come from. Who would have thought that salvation from cancer might arrive on the wings of a wasp?

