The insect world harbors some of the most sophisticated chemical weapons ever evolved. These tiny creatures produce neurotoxins so precise and powerful that they can shut down predators hundreds of times their size within seconds. What’s even more remarkable is that these same compounds might hold the key to treating some of humanity’s most challenging neurological disorders. From the sting of a solitary wasp to the bite of a huntsman spider, nature has crafted molecular tools that could revolutionize medicine or potentially be weaponized in ways we’re only beginning to understand.
The Evolutionary Arms Race Behind Neurotoxin Development

For millions of years, insects and arachnids have been locked in an evolutionary arms race that makes human military technology look primitive. These creatures have developed neurotoxins not just for defense, but as sophisticated hunting tools that can paralyze prey while keeping the meat fresh for consumption. The precision of these biological weapons is staggering – many target specific ion channels in nerve cells with surgical accuracy.
Take the emerald jewel wasp, which delivers a cocktail of neurotoxins directly into a cockroach’s brain. This isn’t random chemical warfare – it’s a precise neurological intervention that turns the roach into a compliant zombie. The wasp’s venom targets specific regions of the brain responsible for motivation and escape reflexes, essentially performing microsurgery with molecular scalpels.
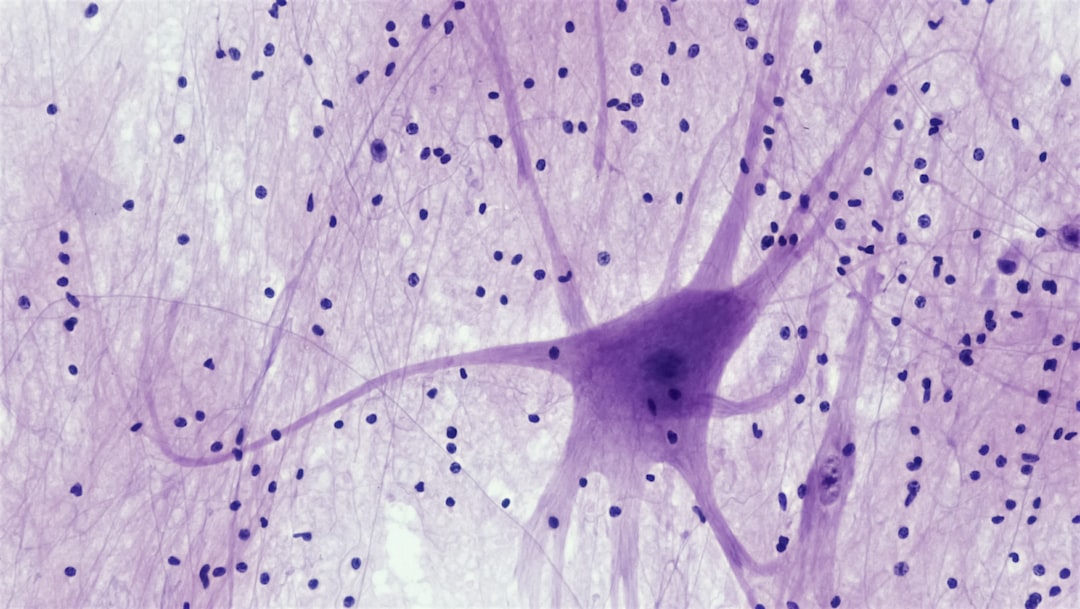
What makes these toxins particularly fascinating is their selectivity. Unlike crude poisons that cause widespread damage, insect neurotoxins often target single types of nerve channels. This specificity means they can shut down motor function while leaving sensory systems intact, or block pain signals without affecting consciousness.
Spider Venom: Nature’s Most Sophisticated Pharmacy

Spiders produce some of the most complex neurotoxins in the animal kingdom, with some species manufacturing over 3,000 different compounds in their venom glands. The Sydney funnel-web spider’s venom contains a peptide called atracotoxin, which binds to sodium channels in nerve cells and causes them to fire uncontrollably. This creates a cascade of electrical chaos that can shut down the entire nervous system.
Recent research has revealed that spider venoms contain molecules that could treat chronic pain, epilepsy, and even stroke damage. The Chilean rose tarantula produces a compound that blocks specific calcium channels involved in pain transmission. Scientists are now working to synthesize modified versions of these molecules that could provide long-lasting pain relief without the addictive properties of opioids.
What’s particularly intriguing is how these toxins have evolved to work across species barriers. A venom that evolved to paralyze insects often affects mammalian nervous systems in similar ways, suggesting fundamental similarities in how nerve cells function across evolutionary lines.
Bee and Wasp Venoms: From Backyard Sting to Medical Breakthrough

The humble honeybee carries a neurotoxin called melittin that could revolutionize treatments for multiple sclerosis and Parkinson’s disease. This compound can cross the blood-brain barrier – a notoriously difficult feat for most medications – and has shown promising results in reducing inflammation in brain tissue. The irony isn’t lost on researchers that an insect most people try to avoid could hold the key to treating devastating neurological conditions.
Paper wasps produce a different class of neurotoxins called mastoparans, which interfere with calcium signaling in nerve cells. These compounds have caught the attention of researchers studying Alzheimer’s disease, as they might help prevent the accumulation of toxic proteins that characterize the condition. The precision with which these toxins target specific cellular processes is remarkable – they can distinguish between healthy and diseased nerve cells.
Social wasps like yellowjackets have evolved venoms that contain both immediate-acting neurotoxins and longer-lasting compounds that continue affecting the nervous system hours after injection. This dual-action approach could inspire new drug delivery systems that provide both immediate relief and sustained therapeutic effects.
Ant Neurotoxins: Small Insects, Massive Chemical Arsenal

Fire ants inject a neurotoxin called solenopsin that creates the characteristic burning sensation of their sting. But beneath this painful experience lies a sophisticated molecular mechanism that researchers are studying for potential medical applications. The toxin works by disrupting cellular membranes and interfering with nerve signal transmission, effects that could be harnessed for treating certain types of cancer.
Bullet ants produce one of the most potent neurotoxins in the insect world – a compound called poneratoxin that causes excruciating pain lasting up to 24 hours. Scientists have discovered that this toxin blocks specific sodium channels in nerve cells, and modified versions might help treat chronic pain conditions by essentially “turning off” pain signals at their source.
Army ants use a different strategy, producing neurotoxins that cause paralysis rather than pain. These compounds could inspire new anesthetics that provide complete muscle relaxation without affecting consciousness or breathing – a holy grail in surgical medicine.
Scorpion Venom: Ancient Neurotoxins for Modern Medicine

Scorpions have been perfecting their neurotoxins for over 400 million years, and this evolutionary refinement shows in the sophistication of their venom. The deathstalker scorpion produces a peptide called chlorotoxin that can specifically target brain tumor cells while leaving healthy tissue unharmed. This remarkable selectivity has led to experimental treatments where the toxin is used to deliver chemotherapy drugs directly to cancerous cells.
Other scorpion species produce neurotoxins that affect different types of ion channels, creating a natural library of molecular tools for manipulating nerve function. The Arizona bark scorpion’s venom contains compounds that could treat epilepsy by preventing the excessive electrical activity that causes seizures. These toxins work by fine-tuning the electrical properties of nerve cells rather than simply blocking all activity.
What makes scorpion neurotoxins particularly valuable is their stability and specificity. Unlike many synthetic drugs that break down quickly in the body, these evolved compounds remain active for extended periods and target their intended cellular mechanisms with remarkable precision.
The Blood-Brain Barrier Problem: How Bug Toxins Break Through
One of the biggest challenges in treating neurological disorders is getting medications past the blood-brain barrier – the body’s natural defense system that prevents most substances from reaching brain tissue. Many insect neurotoxins have evolved specifically to overcome this barrier, making them invaluable templates for drug development. The key lies in their molecular structure, which often mimics natural brain chemicals that the barrier recognizes as safe.
Researchers have discovered that certain spider venom peptides can act as molecular “Trojan horses,” carrying therapeutic compounds across the blood-brain barrier. This discovery has opened new possibilities for treating conditions like brain tumors, stroke, and neurodegenerative diseases that have been notoriously difficult to address with conventional medications.
The mechanisms these toxins use to cross the barrier are as varied as the insects that produce them. Some bind to specific transport proteins, while others temporarily disrupt the barrier’s integrity in highly localized areas. Understanding these natural delivery systems could revolutionize how we approach brain-targeted therapies.
Pain Management Revolution: Learning from Nature’s Anesthetics

The opioid crisis has highlighted the urgent need for new approaches to pain management, and insect neurotoxins offer promising alternatives. Many of these compounds can block pain signals without creating dependency or tolerance, addressing two of the biggest problems with current pain medications. The key difference lies in how they interact with nerve cells – rather than flooding the brain with chemicals that affect mood and consciousness, they target specific pain pathways.
Cone snail venom has already been developed into a prescription pain medication called ziconotide, proving that nature’s neurotoxins can be successfully adapted for human use. Researchers are now looking at similar compounds from various insects and arachnids, seeking to create a new generation of pain relievers that provide effective relief without the devastating side effects of opioids.
The precision of these natural pain blockers is remarkable. Some can distinguish between different types of pain – blocking chronic inflammatory pain while leaving acute warning pain intact. This selectivity could lead to treatments that eliminate suffering while preserving the body’s natural protective mechanisms.
Neurological Disorders: Targeting the Root of the Problem
Conditions like multiple sclerosis, Parkinson’s disease, and Alzheimer’s involve complex disruptions of nerve cell function that have proven difficult to treat with conventional medications. Insect neurotoxins offer a different approach – rather than trying to compensate for damaged nerve cells, they could potentially repair or protect the underlying cellular mechanisms. This represents a fundamental shift from managing symptoms to addressing root causes.
The precision with which these toxins target specific cellular processes makes them ideal candidates for treating neurodegenerative diseases. Some compounds can selectively eliminate damaged nerve cells while leaving healthy ones intact, potentially slowing or stopping disease progression. Others can stimulate the growth of new nerve connections, offering hope for repairing brain damage from stroke or injury.
What’s particularly exciting is how these natural compounds often work through multiple pathways simultaneously. While synthetic drugs typically target single mechanisms, insect neurotoxins can address several aspects of neurological disease at once, potentially providing more comprehensive treatment with fewer side effects.
The Dark Side: Potential for Biological Weapons

The same properties that make insect neurotoxins promising for medicine also make them potentially dangerous as weapons. Their ability to cross the blood-brain barrier and target specific nerve functions could theoretically be exploited to create biological weapons that cause paralysis, confusion, or death. This dual-use potential has led to increased security measures around research involving these compounds.
The threat isn’t entirely theoretical – some military researchers have investigated whether insect neurotoxins could be weaponized for crowd control or battlefield use. The challenge lies in delivery systems, as most of these toxins are only effective when injected directly into tissue. However, advances in aerosol technology and synthetic biology could potentially overcome these limitations.
International oversight of this research is complicated by the fact that the same studies needed to develop life-saving medications could also inform weapons development. The scientific community faces the challenge of pursuing beneficial applications while preventing malicious uses of this knowledge.
Synthetic Biology: Engineering Enhanced Neurotoxins
Scientists are no longer limited to using neurotoxins exactly as nature designed them. Modern synthetic biology techniques allow researchers to modify these compounds, enhancing their beneficial properties while reducing unwanted effects. This could lead to “designer neurotoxins” that are more effective, longer-lasting, or more selective than their natural counterparts.
The process involves identifying the specific parts of a neurotoxin molecule responsible for its therapeutic effects, then engineering new versions that amplify these properties. For example, researchers might create a modified spider venom peptide that crosses the blood-brain barrier more efficiently or targets cancer cells more selectively. These engineered compounds could be more potent than any natural toxin while being safer for human use.
However, this technology also raises concerns about creating entirely new classes of biological weapons. The ability to design custom neurotoxins with specific properties could potentially be misused to develop compounds that are more dangerous than anything found in nature. This has led to calls for strict oversight of synthetic biology research involving neurotoxins.
Current Clinical Trials: From Lab to Patient
Several insect-derived neurotoxins are currently being tested in human clinical trials, bringing these natural compounds closer to becoming approved medications. A modified version of funnel-web spider venom is being evaluated for treating stroke patients, while compounds from various bee species are being tested for multiple sclerosis and rheumatoid arthritis. These trials represent years of careful research to ensure safety and efficacy.
The results so far have been promising but mixed. Some patients have shown remarkable improvement with minimal side effects, while others have experienced little benefit. This variability is typical of early-stage clinical trials and doesn’t necessarily indicate failure – it often reflects the complexity of neurological disorders and the need for personalized treatment approaches.
What’s particularly encouraging is that serious adverse effects have been rare in these trials. Unlike many synthetic drugs that cause widespread side effects, the precisely targeted nature of insect neurotoxins seems to minimize unintended consequences. This suggests that even if current formulations don’t prove effective, the underlying approach remains sound.
Manufacturing Challenges: Mass-Producing Nature’s Complexity
One of the biggest obstacles to bringing insect neurotoxins to market is the challenge of manufacturing them at scale. These compounds are incredibly complex molecules that are difficult and expensive to produce using traditional chemical synthesis methods. A single neurotoxin might contain hundreds of atoms arranged in precise three-dimensional structures that are essential for biological activity.
Scientists have developed several approaches to this problem, including using genetically engineered bacteria or yeast to produce the toxins, and creating synthetic versions that maintain the essential features while being easier to manufacture. Some researchers are even exploring the possibility of “farming” venomous insects to harvest their toxins directly, though this approach faces obvious logistical challenges.
The cost of production remains a significant barrier. While a single dose of an insect-derived medication might cost hundreds or thousands of dollars to produce, this could still be cost-effective for treating serious neurological conditions where current treatments are expensive and often ineffective. The key is finding ways to streamline production while maintaining the quality and consistency needed for pharmaceutical use.
Regulatory Hurdles: Navigating the Approval Process

Getting insect neurotoxins approved as medications involves navigating complex regulatory pathways that weren’t designed for these unique compounds. Traditional drug approval processes focus on synthetic molecules with well-understood properties, but neurotoxins derived from venom present novel challenges. Regulators must evaluate not only safety and efficacy but also the consistency of natural products and the potential for contamination.
The regulatory landscape varies significantly between countries, with some being more receptive to natural product-based medicines than others. This has led to a patchwork of approval processes that can delay or complicate the development of these potentially life-saving treatments. Companies developing insect-derived medications must often conduct separate clinical trials for each major market, multiplying costs and development time.
Despite these challenges, regulatory agencies are beginning to develop specialized guidelines for biological products derived from venoms and toxins. This evolution in regulatory thinking reflects growing recognition that these natural compounds represent a valuable and relatively untapped source of new medications.
Future Frontiers: What’s Next in Neurotoxin Research

The field of neurotoxin research is rapidly evolving, with new discoveries being made regularly. Scientists are exploring venoms from previously unstudied species, finding novel compounds with unique properties. Advanced analytical techniques are revealing the precise molecular mechanisms of these toxins, leading to better understanding of how they could be modified for therapeutic use.
Artificial intelligence and machine learning are beginning to play important roles in this research, helping scientists predict which neurotoxins might be most effective for specific conditions and how they might be modified to enhance their therapeutic properties. These computational approaches could dramatically accelerate the development of new treatments by allowing researchers to test thousands of variations virtually before moving to expensive laboratory studies.
The integration of neurotoxin research with other cutting-edge fields like nanotechnology and gene therapy could lead to entirely new approaches to treating neurological disorders. Imagine neurotoxins delivered by microscopic robots that can navigate directly to damaged brain tissue, or gene therapies that cause the body to produce its own therapeutic neurotoxins exactly where they’re needed.
Conclusion

Insect neurotoxins represent millions of years of evolutionary refinement, creating compounds that can manipulate nerve function with surgical precision. As we face growing challenges in treating neurological disorders and managing pain, these natural weapons offer hope for breakthrough treatments that could transform medicine.
The journey from venom to medicine is complex and fraught with challenges. Manufacturing difficulties, regulatory hurdles, and safety concerns all stand between these promising compounds and the patients who might benefit from them. Yet the potential rewards are enormous – treatments for conditions that have resisted conventional therapy, pain relief without addiction, and perhaps even ways to repair damaged nervous systems.
The dual nature of these compounds – their potential for both healing and harm – reminds us that scientific progress requires careful consideration of consequences. As we unlock the secrets of insect neurotoxins, we must ensure that this knowledge serves humanity’s best interests while guarding against misuse. The next time you encounter a spider in your garden or dodge a bee near a flower, remember that these small creatures might be carrying the keys to treating some of humanity’s most challenging medical conditions.

