The complex relationship between humans and insects dates back millennia, with interactions ranging from beneficial pollination to painful encounters that trigger our immune systems. Each year, millions of people worldwide experience adverse reactions to insect stings and bites, ranging from mild irritation to life-threatening anaphylaxis. Understanding these reactions is crucial not only for medical professionals but for anyone who spends time outdoors. This article explores the science behind insect reactions in humans, identifying common culprits, explaining how our bodies respond, and offering guidance on prevention and treatment options for various severity levels.
The Science Behind Insect Allergies

When an insect stings or bites a human, it introduces foreign proteins and toxins into the body that can trigger an immune response. For most people, this response is localized and relatively mild, producing redness, swelling, and itching at the site. In allergic individuals, however, the immune system dramatically overreacts to these substances, treating them as dangerous invaders. This overreaction occurs because the immune system produces antibodies called Immunoglobulin E (IgE) that bind to allergy-triggering substances (allergens) from the insect venom or saliva. When someone is re-exposed to the same allergen, these IgE antibodies recognize it and signal immune cells to release chemicals like histamine, causing inflammation and allergy symptoms that can affect the entire body.
Common Stinging Insects and Their Venom

Hymenoptera insects—including bees, wasps, hornets, yellow jackets, and fire ants—are responsible for most significant allergic reactions to stings in humans. Honeybees have barbed stingers that often remain in the skin, continuing to pump venom even after the bee has flown away. Wasps and hornets, by contrast, have smooth stingers that allow them to sting repeatedly without losing their stinging apparatus. Yellow jackets are particularly aggressive and commonly sting humans during outdoor activities involving food. Fire ants don’t technically “sting” but rather bite to grip the skin, then pivot their bodies to inject venom multiple times, creating a characteristic circular pattern of pustules. The venom composition varies among species but typically contains proteins, enzymes, and bioactive amines that can cause both local tissue damage and systemic reactions.
Biting Insects and Allergic Responses

While stinging insects inject venom defensively, biting insects feed on human blood and inject saliva containing anticoagulants and anesthetic compounds to facilitate their meal. Mosquitoes are perhaps the most common culprits, affecting nearly everyone with their characteristic itchy welts caused by proteins in their saliva. Bed bugs create distinctive line patterns of bites and can cause significant psychological distress along with physical symptoms. Ticks attach to the skin and feed for extended periods, potentially transmitting diseases like Lyme disease or Rocky Mountain spotted fever. Fleas produce intensely itchy bites often clustered around the ankles and lower legs. Unlike stinging insects, severe allergic reactions to biting insects are less common, though they can still occur in sensitized individuals.
Types of Reactions: From Normal to Severe

Human reactions to insect stings and bites exist on a spectrum of severity, with four main categories typically recognized by medical professionals. Normal or localized reactions involve pain, redness, swelling, and itching confined to the area around the bite or sting, typically resolving within hours or days. Large local reactions extend beyond the immediate sting site, sometimes affecting an entire limb with significant swelling that peaks at 48 hours and can persist for up to a week. Systemic non-anaphylactic reactions affect parts of the body beyond the sting site but don’t threaten breathing or blood pressure, with symptoms like widespread hives, swelling, nausea, or vomiting. The most dangerous category, anaphylaxis, represents a severe, potentially life-threatening allergic reaction characterized by respiratory distress, dramatic blood pressure drops, lightheadedness, and loss of consciousness that requires immediate emergency treatment.
Recognizing Anaphylaxis: When Minutes Matter

Anaphylaxis represents the most severe allergic reaction to insect stings or bites and requires immediate recognition and treatment. Early symptoms often include sudden anxiety, widespread hives, flushing, and intense itching of the skin. As the reaction progresses, the individual may experience swelling of the tongue and throat, difficulty breathing, chest tightness, and a sensation of impending doom. The cardiovascular system becomes involved as blood pressure drops dramatically, leading to dizziness, weakness, and potentially loss of consciousness. Gastrointestinal symptoms like cramping abdominal pain, vomiting, and diarrhea can also occur. These symptoms typically develop rapidly, often within minutes of the sting, though some reactions can be delayed by 30 minutes or occasionally longer, making vigilant observation crucial after any sting in susceptible individuals.
Risk Factors for Severe Reactions

Certain factors significantly increase the risk of experiencing severe allergic reactions to insect stings and bites. Previous allergic reactions to insect stings represent the most significant predictor, with each subsequent exposure potentially triggering more severe responses. Age plays a complex role, with both very young children and older adults facing higher risks of severe outcomes, though for different physiological reasons. Underlying cardiovascular diseases can compromise the body’s ability to compensate during anaphylaxis. Medications like beta-blockers and ACE inhibitors, commonly prescribed for heart conditions and hypertension, can both increase reaction severity and interfere with emergency treatments. Mastocytosis, a rare condition involving an abnormal accumulation of mast cells (key players in allergic reactions), dramatically increases the risk of severe reactions even to mild environmental triggers like insect stings.
Diagnosing Insect Allergies

Accurate diagnosis of insect allergies typically begins with a detailed medical history, including discussion of previous reactions, their severity, and circumstances surrounding the events. Skin testing represents the gold standard for identifying specific insect allergies, involving the placement of small amounts of insect venom on pricked or scratched skin, with a positive reaction producing a wheal and flare response within 15-20 minutes. For patients with skin conditions or those taking medications that interfere with skin tests, blood tests measuring specific IgE antibodies against various insect venoms provide an alternative diagnostic approach. Component-resolved diagnostics (CRD), a newer testing method, can identify antibodies to specific proteins within venoms, helping distinguish between true allergies and cross-reactions. In unclear cases, challenge tests may be conducted in specialized medical settings where patients are exposed to gradually increasing amounts of venom under close supervision to confirm diagnosis.
Treatment Options for Insect Reactions
Treatment approaches for insect reactions vary based on the severity of symptoms and individual patient factors. For mild local reactions, over-the-counter antihistamines like diphenhydramine or cetirizine can reduce itching and swelling, while ice packs and elevation help manage discomfort. Larger local reactions may benefit from oral corticosteroids like prednisone to reduce inflammation. For severe allergic reactions or anaphylaxis, epinephrine (adrenaline) administered via auto-injector is the first-line treatment, working rapidly to constrict blood vessels, relax airway muscles, and stabilize blood pressure. Patients with known severe insect allergies should carry epinephrine auto-injectors at all times and seek immediate emergency care after using them, as additional medications and monitoring are often necessary. For long-term management, venom immunotherapy (allergy shots) can desensitize the immune system over time, reducing the risk of future severe reactions by up to 98% in properly selected patients.
Prevention Strategies for the General Population

Preventing insect stings and bites begins with understanding insect behavior and modifying environments to reduce encounters. When outdoors, avoid wearing bright colors and floral patterns that may attract stinging insects, and minimize the use of scented products including perfumes, colognes, and scented sunscreens. Cover food and drinks promptly, especially sweet items and alcoholic beverages that particularly attract yellow jackets and other wasps. Wear appropriate clothing for outdoor activities, including closed-toe shoes, long pants, and long-sleeved shirts when in areas with high insect activity. Apply EPA-registered insect repellents containing DEET, picaridin, IR3535, or oil of lemon eucalyptus to exposed skin, following product instructions carefully, especially for children. Around homes, eliminate standing water where mosquitoes breed, keep garbage containers tightly sealed, and promptly repair damaged window screens to create barriers against unwanted insect entry.
Additional Precautions for Allergic Individuals

People with confirmed insect allergies must take extra precautions beyond general preventive measures to minimize exposure risks. Medical identification jewelry clearly stating the specific insect allergy should be worn at all times to inform first responders in case of a reaction when the person cannot communicate. Develop and regularly review an emergency action plan with family members, friends, coworkers, and school personnel, ensuring everyone understands how to recognize anaphylaxis and administer epinephrine if needed. Carry at least two epinephrine auto-injectors at all times, checking expiration dates regularly and understanding proper storage requirements to maintain medication effectiveness. Consider consulting with an allergist about venom immunotherapy, particularly for those with histories of systemic reactions, as this treatment significantly reduces the risk of future severe reactions. Inform outdoor event hosts, travel companions, and activity leaders about the allergy to ensure appropriate support in high-risk environments.
Managing Psychological Aspects of Insect Allergies

The psychological impact of severe insect allergies often extends beyond physical symptoms, affecting quality of life through anxiety, hypervigilance, and activity restriction. Many individuals with insect allergies develop entomophobia (fear of insects) or specific phobias related to their allergen, sometimes leading to avoidance behaviors that significantly limit outdoor activities and social engagement. Parents of allergic children frequently experience heightened anxiety, sometimes transferring these fears to their children through overprotective behaviors. Cognitive-behavioral therapy has shown effectiveness in addressing these psychological aspects, helping individuals develop realistic risk assessments and coping strategies. Support groups, both in-person and online, provide valuable emotional support and practical advice from others facing similar challenges. By addressing both physical and psychological dimensions of insect allergies, comprehensive management improves overall quality of life while maintaining appropriate safety measures.
Global Perspectives and Climate Change Impacts

Insect-related allergies and reactions represent a global health concern with significant regional variations in prevalence, responsible species, and healthcare approaches. In the United States, honeybees, wasps, and fire ants predominate as causes of allergic reactions, while in Australia, jack jumper ants represent a significant source of severe reactions. Asia faces distinctive challenges with giant hornets, particularly the Asian giant hornet (Vespa mandarinia), whose venom contains potent neurotoxins. Climate change is dramatically altering insect distributions worldwide, with warming temperatures allowing species to expand into previously inhospitable regions. For example, fire ants continue spreading northward in the United States, while disease-carrying mosquito species extend their ranges into temperate regions. These shifting patterns create new exposure risks for previously unexposed populations and challenge public health systems to adapt surveillance, prevention, and treatment approaches to evolving threats.
Emerging Research and Future Directions

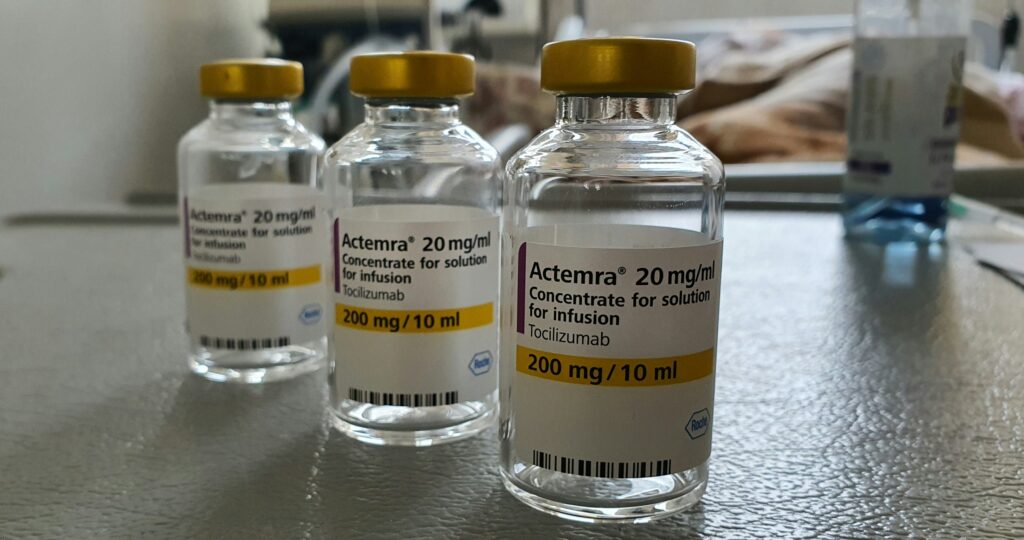
The field of insect allergy is witnessing exciting research advances that promise to transform diagnostic and treatment approaches in coming years. Component-resolved diagnostics are becoming increasingly refined, allowing for personalized risk assessment based on individual sensitivity profiles to specific venom proteins rather than crude venom extracts. Novel biomarkers that predict reaction severity are under investigation, potentially allowing clinicians to identify high-risk patients before they experience severe reactions. Alternative immunotherapy protocols, including rush and ultra-rush desensitization, compress traditional treatment timelines from years to weeks or even days, improving patient adherence while maintaining safety profiles. Molecular-based approaches targeting specific immunological pathways are in development, with biologics like anti-IgE therapies showing promise as adjuncts to conventional treatments. Additionally, research into stable, heat-resistant epinephrine formulations could eventually eliminate the strict storage requirements of current auto-injectors, particularly benefiting regions with limited refrigeration access.
Conclusion
Understanding insect reactions—from mild local responses to life-threatening anaphylaxis—empowers individuals to navigate the outdoors safely while managing risk appropriately. Through accurate diagnosis, proactive prevention, and prompt treatment, most people with insect allergies can maintain active lifestyles with minimal limitations. As climate change alters insect distributions and medical research advances treatment options, staying informed about both established practices and emerging approaches becomes increasingly important. Whether you’re an outdoor enthusiast, a concerned parent, or someone managing a newly diagnosed insect allergy, comprehensive knowledge about these fascinating yet potentially dangerous interactions between humans and insects provides the foundation for confidence and safety in our shared environment.

